Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Prolonged High Output Non-Chylous Lymphatic Drainage in A Post-Pancreaticoduodenectomy -An Unusual Case Report
*Corresponding author:Balaji Prasad Mohanakrishnan MD, Internal Medicine, Texas Tech University Health Sciences, Amarillo, Texas 79124, USA.
Received: March 15, 2022; Published:March 30, 2022
DOI: 10.34297/AJBSR.2022.15.002177
Abstract
Lymphatic leak following pancreaticoduodenectomy has been reported in the literature as chylous leak which occurs in up to 10% of patients [1] whereas non-chylous drainage has not been reported. We report an unusual case of prolonged non-chylous lymphatic drainage after classical Whipple’s pancreaticoduodenectomy for a periampullary carcinoma with obstructive jaundice post ERCP and stenting. Such a drainage causes significant concern to the surgeon and the patient regarding morbidity and nutrition but can be safely managed conservatively with drain in-situ, though for a prolonged duration than expected and without additional morbidity.
Keywords: Pancreaticoduodenectomy, Non-Chylous Leak, Lymphatic Drainage.
Abbreviations: FJ: Feeding Jejunostomy; PD: Pancreaticoduodenectomy; PG: Pancreaticogastrostomy; POD: Post Operative Day.
Introduction
Lymphatic leak has been reported following pancreaticoduodenectomy (PD) as chylous leak in 10% of patients [1] whereas non-chylous leak has not been reported. Any leak causes significant concern more so if chylous. We report a case of prolonged non-chylous lymphatic drainage post-pancreaticoduodenectomy as an unusual observation which was managed without surgical intervention leading to uneventful recovery.
Case Presentation
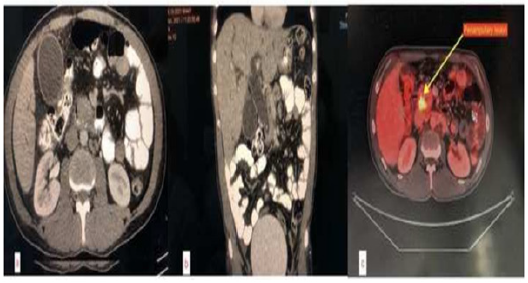
We report a 44-year-old man who presented with complains of jaundice, clay-coloured stools and generalised itching of 15 days duration along with anorexia and weakness. He was evaluated outside with CECT which showed periampullary lesion (Figure 1) and was initially managed with ERCP and plastic CBD stent placement for bilirubin of 23 mg/dl and ampullary biopsy which proved moderately differentiated adenocarcinoma on review at this centre. After relief of jaundice, he was planned for Whipple’s procedure.
On admission for surgery, he was asymptomatic and had no features of cholangitis and his ECOG performance score was 1. An 18-FDG PET/CT scan showed avid lesion in head of pancreas with dilated CBD and IHBRD with stent in-situ (Figure 1). His labs noted with total and direct bilirubin of 3.8 and 2.5 mg/dl respectively, amylase 308 U/L, lipase 3016 U/L. Other hematological and biochemical parameters were within normal limits. His preoperative serum albumin was 2.9 g/dl with AG ratio of 0.6 and was started on high protein diet for optimization for surgery. Through a midline laparotomy approach, the lesion was deemed resectable in standard fashion as described by Evans [2]. Multiple lymph nodes were found in stations 8, 12, periportal and retro duodenal stations with largest node reaching up to 3 cm in size as detected intraoperatively. Complete resection with adequate lymph node dissection was performed by classical Whipple’s procedure (Figure 2). Reconstruction was achieved with duct-to-mucosa pancreatico-gastrostomy (PG), end to side hepaticojejunostomy and end to side gastrojejunostomy. Closure was done over two drains in abdomen - one in lesser sac near pancreatic anastomosis on left side and another in Morrison’s pouch taken out from right side of the abdomen. A feeding jejunostomy (FJ) was created for early postoperative nutritional support. Total operative time was 07 hours and estimated blood loss was 400ml.
On POD2, He developed 400ml clear, non-bilious output from right sided drain unexpectedly as a pancreatic leak was anticipated to drain from the left side. The amylase was detected on from both drains’ fluid, 28 U/L in right side drain and 1200 U/L in left sided drain, although the output of left side drain was only approximately 30 ml per day. Injection Octreotide infusion was started to reduce the output and to keep the drain controlled [3]. However, the right drain output continued to be high and increased up to 1200ml per day by POD7, whereas the left sided drain remained controlled with output of 30 ml per day. Hence the left side drain was removed on POD7.
Repeat amylase was noted to be 6 U/L with negative chylomicrons and creatinine on the right drain fluid ruling out chyle or urine leaks. An ultrasound of the abdomen did not reveal any collection in Morrison’s pouch or any features of pancreatic anastomotic dehiscence. Post-operative nutritional support was adequate with FJ feeds from POD2 and later incremental oral intake from POD7 onwards. The output continued to be high though the patient did not develop any jaundice, haemorrhage, or peritonitis. Drain output reduced spontaneously from POD 10 onwards and reduced to approximately 30 ml/day by POD14. Thereby the right drain was removed.
Histopathological examination revealed periampullary adenocarcinoma, stage pT3aN1 (Stage IIB) and was, therefore, planned for adjuvant chemotherapy. He was discharged after first cycle of adjuvant CAPOX and suture removal on POD21 with full diet tolerated orally.
Discussion
This case is being reported in view of the unusual finding of prolonged postoperative drainage from operated site of PD which was neither pancreatic, biliary, chylous, purulent nor haemorrhagic. Also, there was no decrease in output of the drain with octreotide, though he recovered uneventfully spontaneously with continued conservative management and no active intervention. A lymphatic leak was thus suspected possibly following large lymph nodes dissection at the surgical site.
Conclusion
Literature is scarce on such an unusual event with most of the reports being on most feared pancreatic fistula or chylous leak post pancreatic surgery. This case reflects that extensive LN dissection may cause prolonged drainage without significant consequences except for prolonged hospital stay.
Declarations
Funding (information that explains whether and by whom
the research was supported): Not applicable as patient was
managed at govt hospital free of charges.
• Conflicts of interest/Competing interests (include appropriate
disclosures): Authors have no conflict of interest.
• Ethics approval (include appropriate approvals or waivers):
Not applicable.
• Consent to participate (include appropriate statements):
Written informed consent was taken from the patient.
• Consent for publication (include appropriate statements):
Patient has been informed about publication of his case in a
scientific journal for educational purpose.
• Availability of data and material (data transparency): All data
and material available as hard copy.
• Code availability (software application or custom code): Not
applicable.
• Authors’ contributions: All authors contributed to designing
the report and checking of references.
Acknowledgments
The patient informed consent obtained for publishing of case details and accompanying images.
References
- Strobel O, Brangs S, Hinz U, Tausch T, Hüttner FJ, et al. (2016) Chyle leak after pancreatic surgery: Incidence, risk factors, clinical relevance, and therapeutic implications. Pancreatology 16(3): 1.
- Fischer JE (2019) Mastery of surgery. Wolters Kluwer, Philadelphia.
- Chunli Wang, Xin Zhao, Shengyi You (2017) Efficacy of the prophylactic use of octreotide for the prevention of complications after pancreatic resection: An updated systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore) 96(29): e7500.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.